
Singapore has a compelling health policy story. In a nutshell, the population enjoys excellent health status while public and total expenditures on healthcare remain low. Its achievements look all the more remarkable in comparison to its high income peers in OECD, as shown in the following table:
Table 1. Health expenditures and health outcomes
| High income OECD | Singapore |
| Total health expenditure (% of GDP) | 12.6 | 4.6 |
| Public health expenditure (% of total health expenditure) | 61.4 | 39.8 |
| Life expectancy at birth, total (years) | 80.7 | 82.3 |
| Mortality rate, under-5 (per 1,000) | 5.1 | 2.8 |
Source: World Bank (2016).
International benchmarking lend further credence to Singapore’s fine record. The Economist Intelligence Unit (2014) ranks its health system the second best (after Japan) out of 166 in the world. Similarly, the Bloomberg Health-Care Efficiency Index 2017 ranks it second best among 55 countries.
Like all good stories, there are villains and heroes in the Singapore story: market competition and medical savings account are the heroes that fight off the evils of information asymmetry and moral hazards that are the bane of healthcare systems. The remarkable headline numbers and the accompanying narrative have attracted widespread admiration from commentators around the world in recent years (For example, see Callick 2008; Haseltine, 2013; Gobry 2014; Doutthat 2017).
Alas, if only healthcare policy were so simple. The reality is messy and there is no magic bullet. Singapore’s success in healthcare is built on a panoply of measures developed and refined over decades. The measures employ a variety of policy tools that both individually and collectively target the market and government failures afflict the healthcare sector. For a comprehensive understanding of health policy in Singapore, we need to understand all the policy tools used and how they operate individually and in relation to each other.
 For starters, the Singapore government intervenes heavily and comprehensively in the health sector, especially after the unsatisfactory experience with corporatisation, deregulation and marketisation of the sector in the mid-1980s which saw massive rise in costs and public disquiet (Ramesh, 2008A). The 1993 White Paper, which critically reviewed the 1980s reforms, bluntly noted: “Market forces alone will not suffice to hold down medical costs to the minimum…. In healthcare, supply tends to create its own demand, thus raising healthcare expenditure. The Government therefore needs to intervene to prevent an oversupply of services, to dampen unnecessary demand and ultimately, to control costs” (Government of Singapore, 1993). The report particularly emphasised the need to regulate fees charged by providers and control the supply of hospital beds and physicians. It also boldly addressed the delicate issue of rationing demand: “We cannot avoid rationing medical care, implicitly or explicitly …. To get the most from the limited health budget, we need to exclude treatments which are not sufficiently cost effective to belong to the basic health package available to all.” (Government of Singapore, 1993, p. 24). In the following years, the government refined its health policy interventions that involved vast expansion in the range of tools it employed to manage the sector. The underlying trend in the choice of tools was their focus on addressing specific governance problems rather than promoting the role of the market or the state.
For starters, the Singapore government intervenes heavily and comprehensively in the health sector, especially after the unsatisfactory experience with corporatisation, deregulation and marketisation of the sector in the mid-1980s which saw massive rise in costs and public disquiet (Ramesh, 2008A). The 1993 White Paper, which critically reviewed the 1980s reforms, bluntly noted: “Market forces alone will not suffice to hold down medical costs to the minimum…. In healthcare, supply tends to create its own demand, thus raising healthcare expenditure. The Government therefore needs to intervene to prevent an oversupply of services, to dampen unnecessary demand and ultimately, to control costs” (Government of Singapore, 1993). The report particularly emphasised the need to regulate fees charged by providers and control the supply of hospital beds and physicians. It also boldly addressed the delicate issue of rationing demand: “We cannot avoid rationing medical care, implicitly or explicitly …. To get the most from the limited health budget, we need to exclude treatments which are not sufficiently cost effective to belong to the basic health package available to all.” (Government of Singapore, 1993, p. 24). In the following years, the government refined its health policy interventions that involved vast expansion in the range of tools it employed to manage the sector. The underlying trend in the choice of tools was their focus on addressing specific governance problems rather than promoting the role of the market or the state.
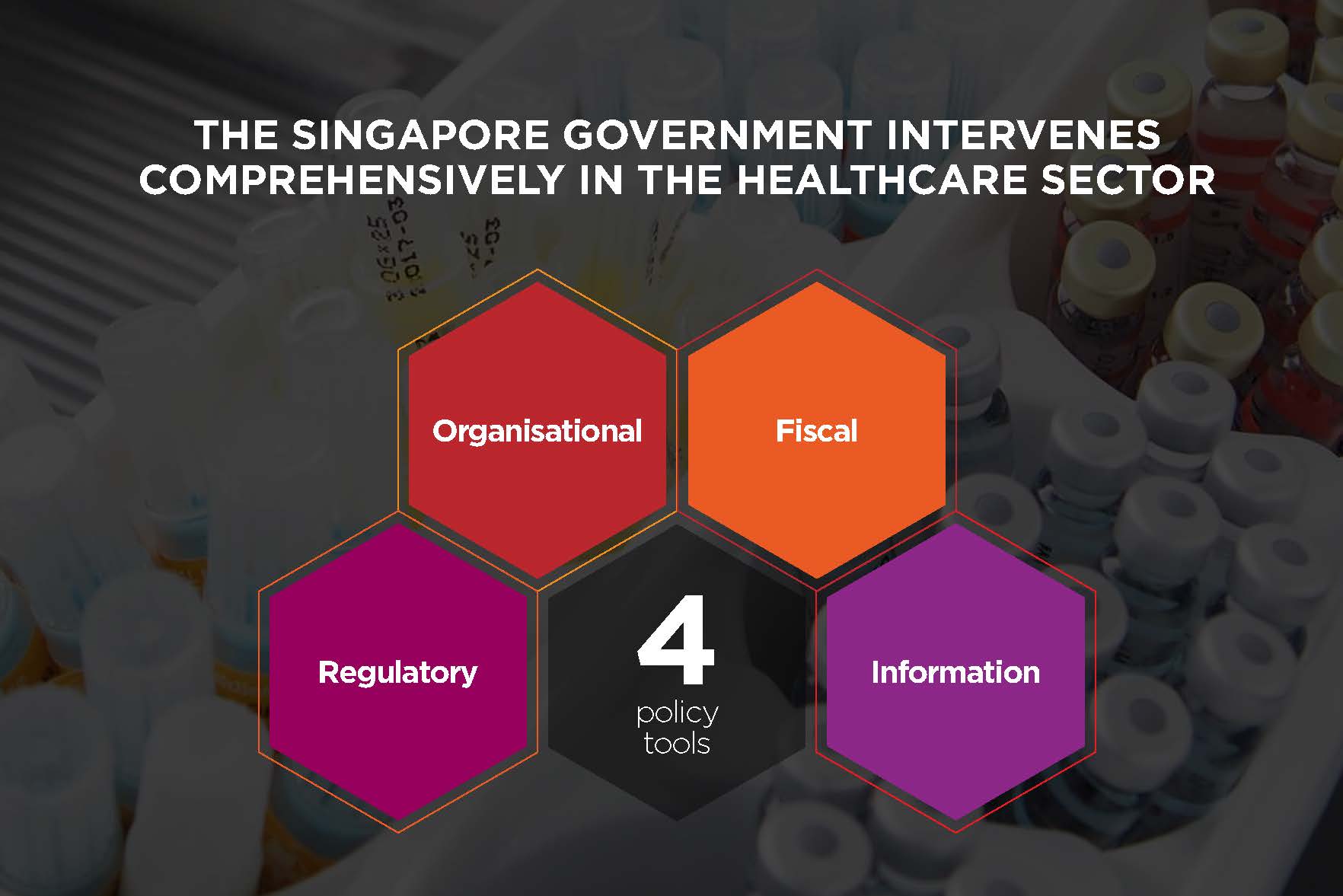 The policy tools currently used to manage the healthcare sector in Singapore are summarised in Figure 1. The tools include a variety of regulatory, organisational, fiscal, and information tools with the Ministry of Health (MOH) at the helm. Collectively, they form a counterweighing system of incentives and disincentives that encourage the key stakeholders to pursue cost-effectiveness, make prudent economic decisions without compromising the overall policy goals of providing necessary healthcare to all at affordable costs.
The policy tools currently used to manage the healthcare sector in Singapore are summarised in Figure 1. The tools include a variety of regulatory, organisational, fiscal, and information tools with the Ministry of Health (MOH) at the helm. Collectively, they form a counterweighing system of incentives and disincentives that encourage the key stakeholders to pursue cost-effectiveness, make prudent economic decisions without compromising the overall policy goals of providing necessary healthcare to all at affordable costs.
Figure 1. Policy tools in Singapore’s healthcare system
| Organisation - Public ownership of Hospitals
- Active Management of Hospitals
- Competition among hospitals
| Fiscal - Subsidy to Public Hospitals
- Medisave, Medifund, and Medishield
- Out-of-pocket payments
|
| Regulation - Close monitoring of all significant aspects of providers’ operations
- Active regulation of providers
| Information - Publishing prices, bill sizes, and clinical outcomes
- Public Campaigns
|
Organisational Tools
 A distinct feature of Singapore’s health system is the overwhelming dominance of the government in hospital ownership, with public hospitals accounting for more than four-fifths of all hospital beds in the country.
A distinct feature of Singapore’s health system is the overwhelming dominance of the government in hospital ownership, with public hospitals accounting for more than four-fifths of all hospital beds in the country.
Similar to many other countries, Singapore began reforming its public hospitals in the mid-1980s in the face of mounting public expenditures on health. Pursuing cost reduction through enhanced efficiency, the reforms promoted competition among hospitals and operational autonomy for managers. Competition was also intended to promote customer-focus, as public hospitals were viewed unfavourably by users.
The award of autonomy to public hospitals and competition among them did indeed improve service quality and cleared surgery backlogs but it also increased costs and reduced affordability (Ramesh, 2008A). The adverse trends led the government in the 1990s to intervene in all significant aspects of hospitals’ operations, their autonomy notwithstanding: the types and volume of specialised clinical services they provide, the fees they charge, the salaries they pay, and the expensive equipment they purchase. It also tweaked the formula by which it paid hospitals, to ensure that hospitals did not under- or over-supply services.
In 1999, the government established two similarly sized “clusters” of vertically integrated public hospitals and clinics. The reorganisation was intended to promote economies of scale, effective coordination and planning of resources, better integration of inpatient and outpatient facilities, and a more effective patient referral system within each cluster. Notwithstanding government ownership, each public hospital is a legally autonomous entity registered as a private firm. Legally, they enjoy operational autonomy in all areas, including recruitment, remuneration, purchase, and pricing of services. They also have substantial revenues and surplus from treating patients in non-subsidised wards which reinforces their autonomy. Yet the fact that the government remains the owner means that it can control and direct them, if necessary, in ways not possible if they were truly private firms. Inspired by the success of two competing clusters, and seeking to further enhance competition, in 2015 all public hospitals and associated polyclinics were reorganised as 6 regional clusters spread across the island.
“Public ownership of what are legally private firms allows hospitals the autonomy they need to operate in a competitive environment and yet be within the government’s direct reach.”
Public ownership of what are legally private firms allows hospitals the autonomy they need to operate in a competitive environment and yet be within the government’s direct reach (Ramesh, 2008B). It provides the government a channel for receiving market feedback and a tool for controlling hospitals’ behaviour. As an owner, the government can shape hospitals’ behaviour without having to resort to onerous regulations or purchase negotiations that would be necessary if they were truly private firms. This has been particularly useful for controlling user charges, physicians’ remunerations, and the number of hospital beds in different ward classes, for instance
Fiscal Tools
 Tax financing for healthcare in Singapore consists of two components: transfers to public hospitals to subsidise the costs of care for patients who do not pay the full costs of treatment, and tax exemptions for Medisave contributions (Tan et al 2014). Such transfers account for 25 per cent of total health expenditure and 70 per cent of the government’s health expenditure (Ramesh 2008A). The government pays public hospitals on the basis of case-mix (diagnosis-related groups or DRGs) as well as block grants. In the 1990s when the formula for grants was changed from block grants based largely on historical figures to fee-for-service, hospitals predictably increased the quantity of services they provided. As a result, in 1999 the government introduced case-mix funding to create incentives for hospitals to make better use of resources. To prevent under-servicing – a problem innate to case-mix because providers are paid a fixed amount per case regardless of the services they provide – the government subsequently moved to a hybrid system, comprising both block funding and case-mix payment (Khaw 2005).
Tax financing for healthcare in Singapore consists of two components: transfers to public hospitals to subsidise the costs of care for patients who do not pay the full costs of treatment, and tax exemptions for Medisave contributions (Tan et al 2014). Such transfers account for 25 per cent of total health expenditure and 70 per cent of the government’s health expenditure (Ramesh 2008A). The government pays public hospitals on the basis of case-mix (diagnosis-related groups or DRGs) as well as block grants. In the 1990s when the formula for grants was changed from block grants based largely on historical figures to fee-for-service, hospitals predictably increased the quantity of services they provided. As a result, in 1999 the government introduced case-mix funding to create incentives for hospitals to make better use of resources. To prevent under-servicing – a problem innate to case-mix because providers are paid a fixed amount per case regardless of the services they provide – the government subsequently moved to a hybrid system, comprising both block funding and case-mix payment (Khaw 2005).
In addition to subsidies at public hospitals, there are many ad-hoc tax-financed schemes. Community Health Assistant Schemes, for instance, is a income-tested scheme that offers additional grants to low-income household for outpatient treatment. Similarly, Pioneer Generation Package subsidises insurance premiums as well as reduces co-payments for elderly Singaporeans. There are also public health campaigns fully financed by the government.
In 1984, Singapore established Medisave, which was then considered an unconventional financing scheme based on compulsory savings. The government’s objective in launching the scheme was to encourage individual responsibility for healthcare, while reducing the government’s fiscal responsibility (Taylor and Blair, 2003). After an episode of hospitalisation, the patient is issued with an itemised bill which can be settled directly from balances in an individual’s Medisave account, subject to a co-payment of 20 percent paid out of pocket (OOP), in addition to daily and annual limits on withdrawal. The mandatory nature of Medisave and restrictions on what it can be used for has resulted in relatively large accumulated balances: total Medisave balances amounted to S$70 billion or equivalent 18 percent of GDP in 2015. However, after more than three decades of operation and a comparatively high contribution rate, Medisave forms less than 10 percent of total healthcare spending (Government of Singapore, 2015).
 Medishield, introduced in 1990 and replaced by Medishield Life in 2015, is a low-cost and basic health insurance scheme for catastrophic hospital costs. It was introduced after realisation that Medisave was insufficient to pay large hospital bills. It is a voluntary scheme (with an opt-out provision) intended to cover those up to the age of 92 years, though new enrolment is not allowed after the age of 75 years. The premiums vary by age and are subsidised based on the income. Thus, the annual premium for Medishield, for example, ranges from $50 for those under the age of 20 years to $1,190 for those between the age of 84 and 85. For patients seeking more generous cover or treatment in upper class hospital wards, additional cover may be purchased from authorised private insurance schemes. The premium for Medishield can be paid from Medisave accounts. There are high deductibles ($1,000 per year for a Class C ward and $1,500 for other wards) and co-insurance requirements (10–20% of the hospital bill). In March 2015, Medishield covered 3.6 million individuals and spending through formed less than 5 percent of total healthcare spending.
Medishield, introduced in 1990 and replaced by Medishield Life in 2015, is a low-cost and basic health insurance scheme for catastrophic hospital costs. It was introduced after realisation that Medisave was insufficient to pay large hospital bills. It is a voluntary scheme (with an opt-out provision) intended to cover those up to the age of 92 years, though new enrolment is not allowed after the age of 75 years. The premiums vary by age and are subsidised based on the income. Thus, the annual premium for Medishield, for example, ranges from $50 for those under the age of 20 years to $1,190 for those between the age of 84 and 85. For patients seeking more generous cover or treatment in upper class hospital wards, additional cover may be purchased from authorised private insurance schemes. The premium for Medishield can be paid from Medisave accounts. There are high deductibles ($1,000 per year for a Class C ward and $1,500 for other wards) and co-insurance requirements (10–20% of the hospital bill). In March 2015, Medishield covered 3.6 million individuals and spending through formed less than 5 percent of total healthcare spending.
Medifund was established as a means-tested scheme in 1993 to fill the gaps left by Medisave and Medishield. In the absence of risk pooling and cross-subsidisation, those with low life-time incomes or the poor accumulate lower balances in their Medisave account, which in turn determines their access to medical services. Medifund caters to those who do not have the means to pay for their health bills from OOP or Medisave or Medishield. However, Medifund accounts for a negligible share of total healthcare expenditure as the means test is onerous. In 2014, S$133 million were distributed amongst 766,000 applicants, an average of about S$170 per applicant.
OOP payments are large in Singapore, and is an outcome of deliberate policy design. There is almost no entirely free healthcare in Singapore: everyone is expected to pay all or part of the costs, including hospital care. Outpatient care, including at the polyclinics, is funded largely OOP. The adverse effects of OOP are mitigated by lower prices at government owned and operated polyclinics due to economies of scale and cost-cutting management practices. The lower prices at government clinics have the flow-on effect of driving down prices at private clinics to whom they pose latent competition.
Regulatory Tools
 A key feature of Singapore’s healthcare system is the tight control over access to services. To achieve this, policymakers rely on both demand and supply-side controls to encourage patients and providers to be judicious and cost conscious in their use of healthcare services. For instance, Medishield covers hospitalisation only in basic hospital wards, and prices increase steeply if patients seek treatment in higher class wards, as subsides decline with the ward class, being zero for the highest (i.e. the most comfortable) Class A ward. Similarly, access to advanced tertiary care or diagnostic tests is rationed by waiting times if treatment is to be reimbursed by Medisave and Medishield. While patients have immediate access to tertiary hospitals and specialists, they do not receive subsidised prices in the absence of referrals. Restrictions on the use of Medisave as well as ceilings on the maximum amount that providers can be paid from an individuals Medisave account reduce the malfeasance associated with moral hazard. The MOH is known to closely monitor billing practices of hospitals and raises alarms when it observes anomalies or suspected excessive treatment.
A key feature of Singapore’s healthcare system is the tight control over access to services. To achieve this, policymakers rely on both demand and supply-side controls to encourage patients and providers to be judicious and cost conscious in their use of healthcare services. For instance, Medishield covers hospitalisation only in basic hospital wards, and prices increase steeply if patients seek treatment in higher class wards, as subsides decline with the ward class, being zero for the highest (i.e. the most comfortable) Class A ward. Similarly, access to advanced tertiary care or diagnostic tests is rationed by waiting times if treatment is to be reimbursed by Medisave and Medishield. While patients have immediate access to tertiary hospitals and specialists, they do not receive subsidised prices in the absence of referrals. Restrictions on the use of Medisave as well as ceilings on the maximum amount that providers can be paid from an individuals Medisave account reduce the malfeasance associated with moral hazard. The MOH is known to closely monitor billing practices of hospitals and raises alarms when it observes anomalies or suspected excessive treatment.
Singapore Medical Council, a statutory board under the MOH regulates and licenses healthcare providers in Singapore. The Council plays an active role in ensuring that costs are ‘competitively priced’ and in the stewardship of the sector. There have been instances where the Council has censured providers for ‘over-charging’ patients (Straits Times, 2015). Such controls on provider behaviour reduce their monopoly power in the health sector, and reduce room to engage in maleficent behaviour.
Information Tools
 To take advantage of modern information technologies available for hospital management, the government has encouraged hospital clusters to harmonise their financial, clinical, administrative and diagnostic processes through integrated information systems. All 16 public hospitals use the enterprise software, National Electronic Health Records. However, private hospitals, and more significantly, private clinics continue to resist sharing information with other providers.
To take advantage of modern information technologies available for hospital management, the government has encouraged hospital clusters to harmonise their financial, clinical, administrative and diagnostic processes through integrated information systems. All 16 public hospitals use the enterprise software, National Electronic Health Records. However, private hospitals, and more significantly, private clinics continue to resist sharing information with other providers.
An innovative measure the government has employed to improve service quality and lower prices is to acquire and disseminate information on hospital charges and clinical outcomes. As the Minister of Health put it: “For economics and markets to work, we must make sure that the conditions for market competition exist. That is why I published the bill sizes for the common medical treatments…. When competition is brought to bear on these services, we will then have the right incentives for the healthcare providers to do the right thing, to raise standards even as they reduce cost” (Khaw, 2005). Since 2003, public hospitals have been required to publish their average bill sizes (which includes charges for room, treatment, surgery, laboratory test, etc.) for different common conditions and procedures. The collated data is subsequently published on the MOH’s webpage. Information on the occupancy rates of hospital beds is updated on a weekly basis. Similarly, the Ministry also publishes the distribution of bills across public hospitals for major illnesses. The hospital managers were understandably resistant to disclosing information on their charges and clinical outcomes but the government eventually prevailed over them. Private hospitals were more successful at resisting participation, but many eventually complied due to pressures from the government and users.
Given the volume of data collected over the years, the MOH now maintains online calculators, which are synchronised with Medisave and Medishield limits. Patients may visit the website and estimate the cost of treatment of particular episodes of illness and calculate the share of the bill that may be financed by Medisave and Medishield. Importantly, they can make informed choices on the particular hospital and ward class when they seek treatment, based on their knowledge of average costs and clinical outcomes. The flow of information promoted by government measures mitigates users’ information disadvantage vis-à-vis providers.
Concluding observations
 The first conclusion to emerge from the discussion above is that Singapore’s healthcare achievements are not the result of some magic bullet, Medisave or otherwise. Medisave forms less than a tenth of the country’s total health spending which would make it, prima facie, an unlikely determinant of the system’s outcomes. For a fuller understanding, we need to understand the entire range of policy measures that the government employs and how they target the various failures that afflict the sector.
The first conclusion to emerge from the discussion above is that Singapore’s healthcare achievements are not the result of some magic bullet, Medisave or otherwise. Medisave forms less than a tenth of the country’s total health spending which would make it, prima facie, an unlikely determinant of the system’s outcomes. For a fuller understanding, we need to understand the entire range of policy measures that the government employs and how they target the various failures that afflict the sector.
Furthermore, the case of Singapore shows that policy tools are more effective when used simultaneously and in concert. A concerted use of different tools promote complementarities that are unavailable when they are used in isolation. Take the case of publicly owned and operated hospitals, a typical organisational tool. Instead of running them in traditional command-and-control ways, the Singapore government uses its ownership rights to force them to compete with each other and with private hospitals for users’ funds with the objective of promoting customer focus and operational efficiency on their part. Its ownership also makes it easier for the government to force them to disclose information on costs and clinical outcomes, a requirement vehemently resisted by private hospitals but essential if users are to make informed decisions. Here we see an ingenious combination of public ownership, market competition, and price transparency to achieve different but related objectives. Public ownership also allows the Ministry to directly acquire operational information from public hospitals and respond with appropriate directives as necessary. This is particularly relevant in healthcare as the governance failures are multi-faceted and deeply intertwined and, hence, cannot be addressed in isolation, as policy reformers in many countries have found out (Liang and Langenbrunner, 2013; Ramesh 2013; Bali and Ramesh, 2015b; Harimurti et al 2013).
References
Asher, Mukul G. & Amarendu Nandy. (2006). Health financing in Singapore: A case for systemic reforms, International Social Security Review, 59 (1), pp. 75-92.
Balabanova, D., Oliveira-Cruz, V. &Hanson, K. (2009). Health Sector Governance and Implications for the Private Sector. Washington DC: Results for Development Institute.
Bali, A. S., & Ramesh, M. (2015a). Healthcare reforms in India: Getting it wrong. Public Policy and Administration, 30 (3-4), pp. 300-319.
Bali, A. S., & Ramesh, M. (2015b). Mark Time: India's March to Universal Healthcare Coverage. Social Policy & Administration, 49 (6), pp. 718-737
Bali, A.S. & M Ramesh. (Forthcoming). Designing an Effective Healthcare System: A Policy Tools Approach. Public Administration and Development
Bardach, E. (1980). Implementation Studies and the Study of Implements. Paper presented to the American Political Science Association
Barr, M. D. (2001). Medical savings accounts in Singapore: a critical inquiry. Journal of Health Politics, Policy and Law, 26 (4), pp. 709-726.
Bemelmans-Videc, Marie-Louise, Ray C. Rist, and Evert Vedung, (1998) (Eds.) Carrots, Sticks and Sermons: Policy Instruments and Their Evaluation. New Brunswick: Transaction Publishers.
Blomqvist A (2011) Public sector healthcare financing. In: Glied S and Smith P (eds) The Oxford Handbook of Health Economics. Chippenham: Oxford University Press, pp. 257–284.
Böhm et al, Katharina (2012) Classifying OECD healthcare systems: A deductive approach, TranState Working Papers, No. 165, http://hdl.handle.net/10419/64809.
Bonilla-Chacín, ME. & Aguilera, N. (2013), The Mexican Social Protection System In Health, Washington D.C.: World Bank
Brinkerhoff, D.W., & Bossert, T.J. (2008), Health Governance: Concepts, Experience, and Programming Options, Washington, DC: USAID, Available online http://www.healthsystems2020.org. Accessed 5 August 2011.
Coelho, V., & Shankland, A. (2011), Making The Right To Health A Reality For Brazil's Indigenous Peoples: Innovation, Decentralization And Equity, MEDICC Review, 13 (3), pp. 50-53.
Doremus, H. (2003) “A Policy Portfolio Approach to Biodiversity Protection on Private Lands.” Environmental Science & Policy 6: 217–32.
Elmore, R. F. (1978). Organizational models of social program implementation. Public Policy, 26 (2), pp. 185-228.
Ghesquière, H. C. (2007). Singapore's success: Engineering economic growth. Thomson Learning.
Government of Singapore (1983). National Health Plan: A Blue Paper, Singapore: Ministry of Health.
Government of Singapore (1993). Affordable healthcare: A White Paper, Singapore: Ministry of Health.
Government of Singapore (2015a). “Government Health Expenditure and Healthcare Financing”. Available online at https://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Healthcare_Financing.html
Government of Singapore (2015b) “Ministry Of Health’s 2014 Patient Satisfaction Survey Shows Higher Satisfaction With Public Healthcare Institutions”, Press Release by the Ministry of Health. Available online https://www.moh.gov.sg/content/moh_web/home/pressRoom/pressRoomItemRelease/2015/ministry-of-healths-2014-patient-satisfaction-survey-shows-highe.html (Accessed on September 8, 2015)
Haber, H. 2011. ‘Regulating-for-Welfare: A Comparative Study of ‘‘Regulatory Welfare Regimes’’ in the Israeli, British, and Swedish Electricity Sectors’, Law&Policy, 33, 1, pp. 116–48
Ham, Chris (2001). Values and Health Policy: The Case of Singapore, Journal of Health Politics, Policy and Law, 26: 4, pp. 739-745.
Hanvoravongchai, P. (2013), Health Financing Reform In Thailand: Toward Universal Coverage Under Fiscal Constraints, Washington D.C.:World Bank
Harimurti, P., Pambudi, E., Pigazzini, A., & Tandon, A. (2013), The Nuts & Bolts of Jamkesmas, Indonesia’s Government-Financed Health Coverage Program for the Poor and Near-Poor, Washington DC: World Bank
Haseltine, W. A. (2013). Affordable excellence: the Singapore healthcare story. Brookings Institution Press.
Hood, C. (2007). Intellectual obsolescence and intellectual makeovers: Reflections on the tools of government after two decades. Governance, 20 (1), pp. 127-144.
Hood, Christopher. 1983. The Tools of Government. London: Macmillan.
Howlett, Michael, and Pablo del Rio. (2015). “The Parameters of Policy Portfolios: Verticality and Horizontality in Design Spaces and Their Consequences for Policy Mix Formulation.” Environment and Planning C 33 (5): 1233–45.
Howlett, M., & Rayner, J. (2013). Patching vs packaging in policy formulation: Assessing policy portfolio design. Politics and Governance, 1 (2), pp. 170-182
Howlett, M. (2011), Designing Public Policies: Principles and Instruments, Oxon: Routledge
Howlett, M. (2014). From the ‘old’to the ‘new’policy design: design thinking beyond markets and collaborative governance. Policy Sciences, 47 (3), pp. 187-207.
Howlett, M., & Ramesh, M. (2015). Achilles' heels of governance: Critical capacity deficits and their role in governance failures. Regulation & Governance.doi:10.1111/rego.12091
Howlett, M., M Ramesh, and Anthony Perl (2008) Studying Public Policy, New York: Oxford University Press
Howlett, M., Mukherjee, I., & Woo, J. J. (2015). From tools to toolkits in policy design studies: the new design orientation towards policy formulation research. Policy & Politics, 43 (2), pp. 291-311.
Howlett, Michael, and Raul P. Lejano. (2012): Tales from the crypt: The rise and fall (and rebirth?) of policy design." Administration & Society 0095399712459725.
Hsiao, W. C. (2003), What is a health system? Why should we care? Working Paper. Cambridge: Harvard School of Public Health.
Hsiao, William C. (2001). Behind the Ideology and Theory: What Is the Empirical Evidencefor Medical Savings Account, Journal of Health Politics Policy and Law, 26: 4, pp. 733- 37.
Khaw Boon Wan, (2005). The Best Healthcare that Singaporeans Can Afford, Speech In Parliament, 8 March 2005. http://www.moh.gov.sg/corp/about/newsroom/speeches/details.do?id=30507042
Kirschen, E. S., J. Benard, H. Besters, F. Blackaby, O. Eckstein, J. Faaland, F. Hartog, L. Morissens, and E. Tosco. Economic Policy in Our Time. Chicago: Rand McNally, 1964.
Knaul, F. M., & Frenk, J. (2005), Health Insurance In Mexico: Achieving Universal Coverage Through Structural Reform, Health affairs, 24 (6), pp. 1467-1476.
Kutzin, J., Ibraimova, A., Jakab, M., & O'Dougherty, S. (2009), Bismarck meets Beveridge on the Silk Road: coordinating funding sources to create a universal health financing system in Kyrgyzstan, Bulletin of the World Health Organization, 87 (7), pp. 549-554.
Levi-Faur, David (2014) The welfare state: A regulatory perspective, Public Administration. Public Administration, Vol.92, No.3, pp. 599–614
Liang, L., & Langenbrunner, J. C. (2013), The long march to universal coverage: lessons from China. Washington DC: World Bank
Lim Meng Kin (2002). Singapore’s Medical Savings Accounts — Beyond Rhetoric and Doctrine To "What Works": A Response from Singapore, Journal of Health Politics, Policy and Law, 27: 2, pp. 302-304.
Linder, Stephen H. and B. Guy Peters. “Instruments of Government: Perceptions and Contexts".” Journal of Public Policy. 9, no. 1 (1989): 35-58.
Liu, X. 2003. Policy Tools for Allocative Efficiency of Health Services. Geneva: World Health Organization.
Low, Linda (1998). Healthcare in the Context of Social Security in Singapore, Sojourn, 13: 1: 139.
Lowi, T. J. (1972). Four Systems of Policy, Politics and Choice. Public Administration Review, 32 (4), pp. 298-310.
Marten, R., McIntyre, D., Travassos, C., Shishkin, S., Longde, W., Reddy, S., & Vega, J. (2014), An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS), The Lancet, 384(9960), pp. 2164-2171.
Massaro, Thomas A. and Yu-Ning Wong (1995). Positive Experience With Medical Savings Accounts In Singapore Health Affairs, Summer, pp. 267-272.
McKee, M., & Busse, R. (2013). Medical savings accounts: Singapore’s non-solution to healthcare costs. British Medical Journal, 347, f4797.
Pauly, Mark 1980, Doctors and Their Workshops: Economic Models of Physician Behavior. Chicago: University of Chicago Press for NBER.
Pauly, Mark V. (2001). Savings Accounts in Singapore: What Can We Know? Journal of Health Politics, Policy and Law. 26: 4, pp. 727-731.
Peters, B. Guy and F. K. M. Van Nispen, ed. (1998) Public Policy Instruments : Evaluating the Tools of Public Administration. New York: Edward Elgar, 1998.
Phua Khai Hong (2003). Attacking Hospital Performance on Two Fronts: Network Corporatization and Financing Reforms in Singapore. In A.S. Preker and Harding A. (eds.) Innovations in health service delivery: The corporatization of public hospitals. Washington, DC: The World Bank, pp. 451-484.
Phua, KH and N Pocock (2017) Health and Health Systems in Southeast Asia. Singapore: World Scientific
Preker AS and Langenbrunner JC (2005) Spending Wisely: Buying Health Services for the Poor. Washington, DC: World Bank.
Ramesh, M (2008A) “Competition and Control in Public Hospital Reforms in Singapore, American Review of Public Administration, 38: 1, pp. 62-79.
Ramesh, M. (2008B). Reasserting the role of the state in the healthcare sector: lessons from Asia. Policy and Society, 27 (2), 129-136.
Ramesh, M. (2013), Healthcare reform in Vietnam: Chasing shadows, Journal of Contemporary Asia, 43 (3), 399-412.
Ramesh, M., Wu, X., & He, A. J. (2013), Health governance and healthcare reforms in China, Health Policy And Planning, doi:10.1093/heapol/czs109
Roberts, M., William Hsiao, Peter Berman, and Michael Reich. (2004) Getting Health Reform Right: A Guide to Improving Performance and Equity. New York: Routledge
Ruderman, A. Peter (1988). Health Planning in Singapore: Limits to Privatization, Journal of Public Health Policy, 9: 1, 121-131.
Salamon, Lester M., ed. (2002) The Tools of Government: A Guide to the New Governance. New York: Oxford University Press, 2002.
Savedoff, W. D. (2011), Governance in the Health Sector: A Strategy for Measuring Determinants and Performance, Policy Research Working Paper 5655, Washington DC: World Bank.
Savedoff, W. D., de Ferranti, D., Smith, A. L., & Fan, V. (2012). Political and economic aspects of the transition to universal health coverage, The Lancet, 380 (9845), pp. 924-932.
Schaffrin, André, Sebastian Sewerin, and Sibylle Seubert. (2014). “The Innovativeness of National Policy Portfolios – Climate Policy Change in Austria, Germany, and the UK.” Environmental Politics 23(5): 860–83. doi:10.1080/09644016.2014.924206.
Schneider, Anne, and Helen Ingram. 1990. “Behavioral Assumptions of Policy Tools.” Journal of Politics 52 (2): 510–529.
Somanathan, A., Dao, H.L. and Tien, T.V. (2013), Vietnam Integrating the poor into universal health coverage in Vietnam, Washington, DC: World Bank.
Sovacool, Benjamin K. (2008) “The Problem with the ‘portfolio Approach’ in American Energy Policy.” Policy Sciences 41(3) 245–61. doi:10.1007/s11077-008-9063-1
Straits Times. 2015. “Susan Lim's legal bill rises to $825k as SMC wins appeal”, May 14 2015. Available online at http://www.straitstimes.com/singapore/courts-crime/susan-limslegal-bill-rises-to-825k-as-smc-wins-appeal
Tan KB, Tan WS, Bilger M, Ho CWL (2014) Monitoring and Evaluating Progress towards Universal Health Coverage in Singapore. PLoS Med 11 (9). http://dx.doi.org/10.1371/journal.pmed.1001695
Taylor, Rob and Simon Blair(2003). Singapore’s Innovative Approach Financing Healthcare Singapore’s Innovative Approach HTTP://rru.worldbank.org/viewpoint/index.asp
The Economist Intelligence Unit (2014) Health Outcomes and Costs: A 166 Country Comparsion, Available online at http://www.eiu.com/public/topical_report.aspx?campaignid=Healthoutcome2014 (Accessed January 20, 2015)
Trebilcock, Michael and Douglas G. Hartle. (1982) “The Choice of Governing Instrument.” International Review of Law and Economics, Vol 2, pp. 29-46.
World Bank (2016) World Development Indicators Available online at http://databank.worldbank.org/
Wouters, O. J., Cylus, J., Yang, W., Thomson, S., & McKee, M. (2016). Medical savings accounts: assessing their impact on efficiency, equity and financial protection in healthcare. Health Economics, Policy and Law, 11 (3), pp. 321-335.
Wu, X. and Ramesh, M. (2014), Market imperfections, government imperfections, and policy mixes: policy innovations in Singapore, Policy Sciences, 47, 3: 305–20.
Download
full publication.